
Chicago, IL, May 14, 2025 (GLOBE NEWSWIRE) — “Say the ‘S’ word:” Physician-Patient Alliance for Health & Safety Launches CME Sepsis Courses
Free Three-Module Series Equips Clinicians to Navigate the Sepsis “Gray Zone”
The Physician-Patient Alliance for Health & Safety (PPAHS) is proud to release an accredited continuing medical education course designed to strengthen clinical judgment in the early identification of sepsis. The series is free of charge, self-paced, and completely online.
Sepsis occurs when the body’s inflammatory response to an infection spirals out of control. The symptoms can be subtle, and when left unchecked, they’re deadly: sepsis is the leading cause of death in hospitals, and 1 in 3 septic patients will suffer end-organ damage and die.
Yet due to its vague, murky clinical presentation – which often mimics other conditions – sepsis remains notoriously difficult to identify and diagnose.
This diagnostic uncertainty is the sepsis Gray zone – a term coined by Amy Campbell, Ph.D., RN, CPHQ, LSBB, a Quality Nurse Specialist involved in sepsis research for the last 12 years. In the early, interim stages of sepsis, vital signs may be only slightly abnormal, the source of infection unclear, and often, the patient “just doesn’t seem that sick.”
“It’s not always obvious,” says Dr. Campbell. “It’s so easy to spot on paper when you read a patient chart, but when you’re actually out rounding on patients in real time, it’s much harder.”
The course, Identifying Patients in the Sepsis Gray Zone, was created to close that gap between suspicion and certainty. Thoughtfully designed by leaders in critical care, emergency medicine, and quality improvement – and moderated by Michael Wong, JD, Executive Director of PPAHS – the series reflects the best of current science and clinical humility.
The objective: equip providers, nurses, and allied health professionals with the clarity and clinical insight to spot sepsis early and ultimately save lives.
Through repetition, thoughtful analysis, and realistic case studies, course participants will build the mindset and muscle memory for early detection and timely action. They’ll move beyond rote, automated thinking to integrate clinical insight and gut instinct.
The CME series consists of three modules.
Module 1 – Foundations of Sepsis Diagnosis and the Role of Lactate is a “level-set,” calling clinicians into a shared mindset and language around sepsis detection. This foundational module empowers frontline workers to build a reflex to ask, Could this be sepsis? As Dr. Campbell puts it, this is where the course “teaches people to say the ‘S’ word.”
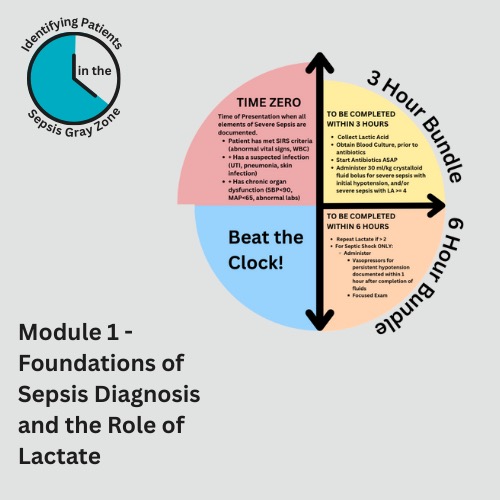
From the physiological cascade to the significance of an elevated lactic acid level, this module revisits what’s happening inside the body – and how every minute counts. In this race against the clock, healthcare professionals will get clear on when “Time Zero” actually begins.
The module also breaks down the rationale behind the Three- and Six-Hour Bundles of sepsis care, so that clinicians understand not just what to do, but why it matters.
Not least, Module 1 highlights the importance of collaboration across the healthcare spectrum, beginning with early detection and chronic disease management in the outpatient setting.
“It takes a multidisciplinary approach to have success for our patients,” explains Jasmine Bonder, DNP, an Acute Care Nurse Practitioner. “Grab the nurse, respiratory therapy, the diabetes specialist – grab everybody – because it takes a village to ensure there are no gaps in care.”
Module 2 – Advances in Sepsis Diagnosis and Clinical Research brings course participants up to speed on the latest clinical trial research. That research is then grounded in unfolding case studies that reflect the complexity of real-world patient care.
Dr. Patrick Cullinan, an ICU and ER physician, leads an important discussion on the evolving role of biomarkers in sepsis diagnosis – as well as their limitations. Biomarkers – lactic acid, procalcitonin, and C-reactive protein, for example – show great promise as tools in the diagnosis of sepsis and the judicious use of antibiotics.
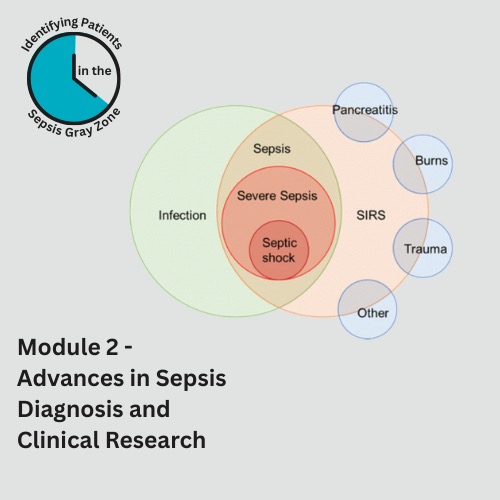
However, context matters. “A fool with a tool is still a fool,” says Dr. Cullinan. “It is critical that you understand how you are using the biomarker and fitting it into your patient’s specific scenario.”
Module 2 teaches the thinking behind the numbers and the protocols, emphasizing that there is no “silver bullet” or “one-size-fits-all” approach to sepsis diagnosis and care. As Dr. Cullinan calls out, “It’s the person in front of me that I want to help, not the population. What’s good for one patient may harm another.”
Module 3 – Navigating the Gray Zone of Sepsis Diagnosis rounds out the arc of the sepsis series and begins with an overview of the SeptiCyte RAPID test, led by pulmonary critical care physician Dr. Robert Balk (Professor, Department of Internal Medicine, Division of Pulmonary, Critical Care and Sleep Medicine, Rush University Medical Center).
In the gray zone of overlapping symptoms, diagnostic ambiguity, and time pressure, the SeptiCyte RAPID can offer timely clarity – in just one hour – by distinguishing sepsis from non-infectious systemic inflammation. This is key in the decision of whether to initiate antibiotics, which improves patient outcomes and fosters antibiotic stewardship.
This final module brings home the message that sepsis diagnosis should be tool-supported but not tool-dependent. “The caution, as with any test, is using it by itself,” explains Dr. Balk. Biomarkers taken together, contextualized by the patient’s overall clinical picture and presentation, “are a stronger predictor of what’s going on than any one standalone test.”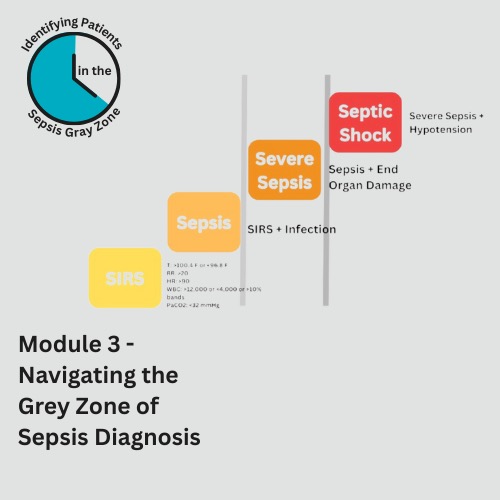 The course concludes with Knowledge In Action: patient scenarios that mirror classical presentations of sepsis. Dr. Adam Bonder, ER physician, guides course participants through the clinical reasoning that narrows down potential sources of infection and drives the selection of the interventions that will be most effective in preventing further decompensation.
The course concludes with Knowledge In Action: patient scenarios that mirror classical presentations of sepsis. Dr. Adam Bonder, ER physician, guides course participants through the clinical reasoning that narrows down potential sources of infection and drives the selection of the interventions that will be most effective in preventing further decompensation.
These stories put a memorable face to vague symptoms, supporting recall and pattern recognition when clinicians encounter similar cases in their practice.
“There is no magic solution to this. There’s nothing that’s going to absolutely point you one way or another,” says Dr. Adam Bonder. “It’s using your judgment and the tools available to you to help define the clinical picture and tailor your approach appropriately to the patient presentation.”
The signs of sepsis may be subtle – but the consequences are not. When early recognition can mean the difference between recovery and decline, Identifying Patients in the Sepsis Gray Zone offers the clarity, confidence, and shared language to act decisively.
The Physician-Patient Alliance for Health & Safety would like to thank Immunexpress and Thermo Fisher Scientific for their educational grants. Because of these grants, PPAHS is able to provide quality clinical educational content at no charge for learners.
Enroll and start learning today here.
About the Physician-Patient Alliance for Health & Safety
Physician-Patient Alliance for Health & Safety is ranked internationally as a top-100 patient safety organization (Agilience Authority Index) and is a national advocacy force for addressing patient health and safety priorities shared by patients, physicians, regulators, and industry. PPAHS seeks to ensure that the best medications, medical inventions, and technology that can improve care and reduce costs are employed. PPAHS works to advance patient health and safety by developing and highlighting best practices and recommendations through better use and application of clinical practices and experiences, information technologies and checklists, and healthcare information. As a voice in support of ideas and innovation that can improve care, we encourage a health ecosystem that fosters a culture of patient safety. For more about PPAHS, please visit www.ppahs.org.
Attachments

Wall St Business News, Latest and Up-to-date Business Stories from Newsmakers of Tomorrow



